We’re working to improve health outcomes and decrease health disparities for vulnerable and underserved populations with type 2 diabetes in the United States. This population is more likely to have diabetes and often experiences barriers to effective management of the disease. We aim to increase access to care and build sustainable partnerships between health care and non-health care sectors.
ESTIMATED PEOPLE IN THE U.S. WITH DIABETES

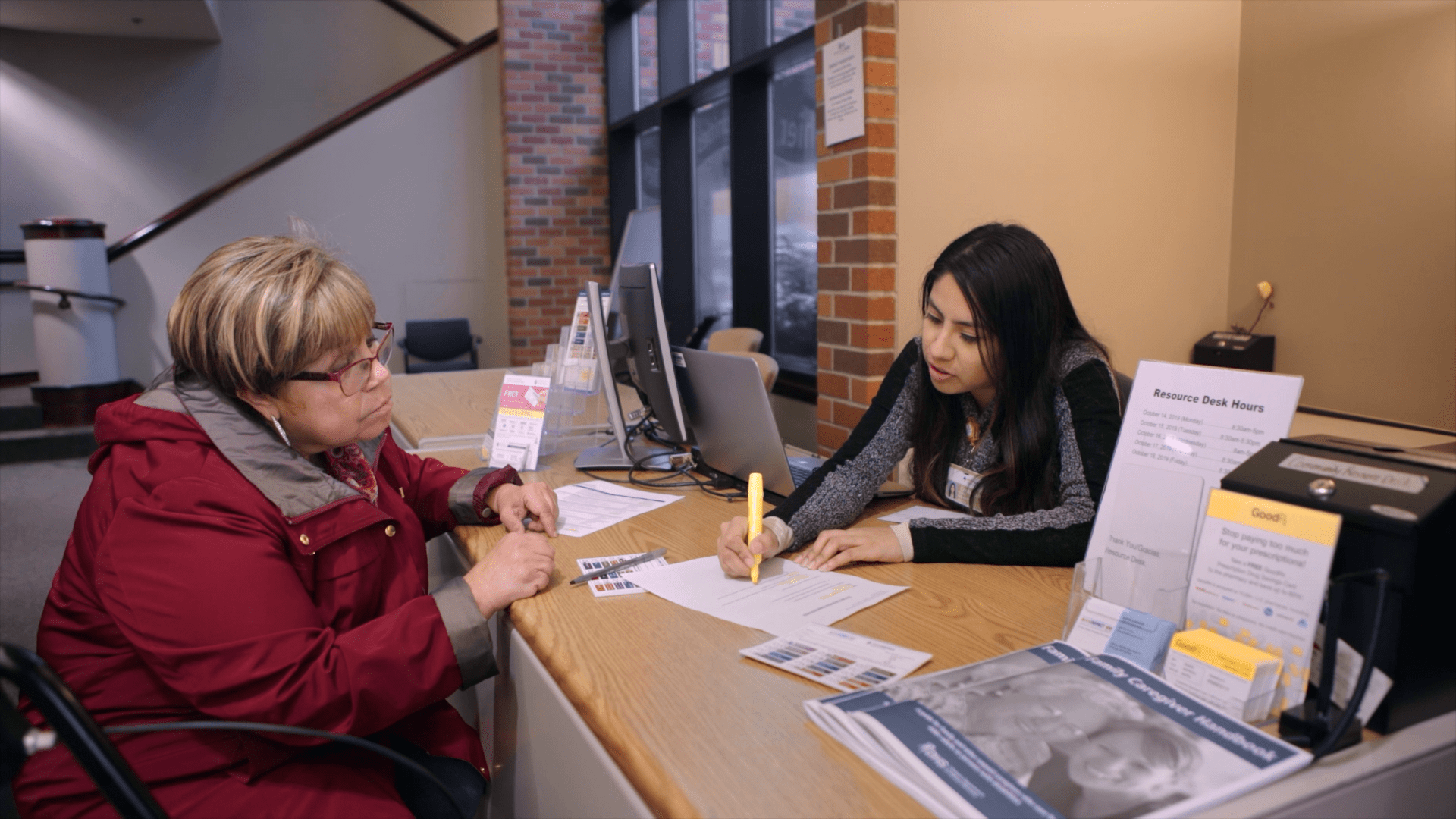
Bridging the Gap: Reducing Disparities in Diabetes Care program partners are implementing comprehensive, evidence-based programs to address the many factors that influence health, such as access to nutritious foods and options for physical activity, housing, and legal services. This collaborative approach between health care and non-health care sectors focuses on improving medical care, and addresses the social and environmental factors that affect vulnerable populations.
Many factors play a role in diabetes care. Bridging the Gap: Reducing Disparities in Diabetes Care partners prioritize strategies to address medical and social needs as part of comprehensive diabetes care. Program partners address medical and social needs through augmented staffing models, information technology innovations, system-wide protocols to identify high-risk populations with gaps in care, and partnership with organizations in other sectors.


Copyright © 2022 — The University of Chicago
